Diabetes mellitus, commonly known as diabetes, is a chronic metabolic disorder that affects millions of people worldwide. Our body breaks down food into glucose, which is then released into the bloodstream. When blood sugar (glucose) levels rise, the pancreas releases insulin, which allows glucose to enter cells for energy use. Diabetes occurs when the body lacks insulin or fails to use it effectively, leading to excessive blood sugar in the bloodstream, which can cause serious health issues like heart disease, vision loss and kidney disease.
Types of diabetes:
Type 1 diabetes:
Type 1 diabetes is an autoimmune condition causing the body to mistakenly attack and destroy insulin-producing cells in the pancreas, often diagnosed in childhood or adolescence but it can develop at any age. Approximately 5-10% of people with diabetes have this condition. To survive, individuals need to take daily insulin injections or an insulin pump. Currently, no known method to prevent type 1 diabetes exists.
Type 2 diabetes:
Type 2 diabetes is a common form of diabetes where the body becomes insulin resistant or fails to produce enough insulin to maintain normal blood sugar levels. It is often linked to a poor diet, lack of exercise, and obesity. It can be managed through lifestyle changes, medication, or insulin therapy. About 90–95% of people with diabetes have type 2 diabetes, which is typically diagnosed in adults but is increasingly prevalent in children, teens, and young adults. It’s crucial to test blood sugar levels if you’re at risk. Preventing or delaying type 2 diabetes can be achieved through weight loss, healthy food consumption, and regular physical activity.
Prediabetes:
Over 1 in 3 US adults have prediabetes, with over 8 in 10 unaware of it. This stage is before Type 2 diabetes, where blood glucose levels are higher than normal but not high enough to be officially diagnosed.
Gestational diabetes:
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet increased needs, leading to elevated blood sugar levels. Controlling this condition is crucial to preventing complications for both the mother and baby. It is more common in pregnant women without diabetes and increases the risk of type 2 diabetes later in life. The baby is more likely to develop obesity as a child or teen.
Symptoms of diabetes:
- Frequent Urination: Increased urination, especially at night.
- Excessive Thirst and Hunger: Constant feelings of thirst and hunger, even after eating.
- Fatigue: Unexplained tiredness and lack of energy.
- Slow Healing: Wounds and cuts take longer to heal.
- Blurred Vision: Vision problems may occur due to high blood sugar levels.
- Tingling or Numbness: Especially in the hands and feet.
- Infections: Getting a lot of infections, such as gum, skin and vaginal infections
Causes of diabetes:
Diabetes is caused by excessive glucose in the bloodstream, with the cause varying depending on the type of diabetes, and each type has unique associated causes,
Type 1 diabetes: Type 1 diabetes occurs when the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas, causing the disease. The exact cause is unknown, but genes may play a role or a virus may trigger an immune system attack.
Type 2 diabetes: Type 2 diabetes is a condition influenced by genetics and lifestyle factors, with overweight individuals being more susceptible to the disease. Insulin resistance, a condition where cells in muscles, fat, and liver don’t respond properly to insulin, is a major contributor. Factors such as obesity, lack of physical activity, diet, hormonal imbalances, genetics, and certain medications contribute to this condition.
Gestational diabetes: Gestational diabetes is a condition resulting from hormonal changes during pregnancy, where the placenta produces hormones that reduce insulin sensitivity, leading to high blood sugar levels. Overweight individuals or those who gain excessive weight during pregnancy are more susceptible to this condition.
How is diabetes diagnosed?
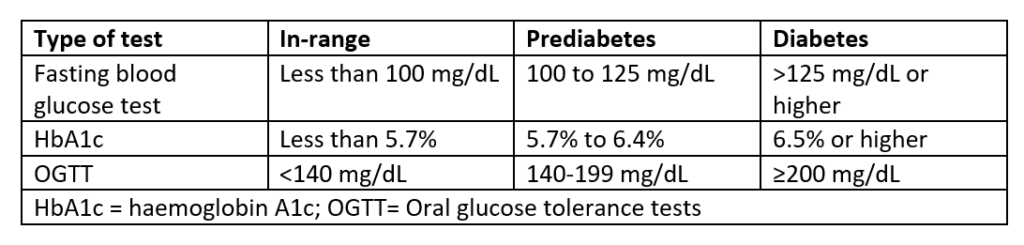
Individuals with diabetes symptoms or risk factors should be routinely tested. Gestational diabetes is typically diagnosed during the second or third trimester of pregnancy. Healthcare providers diagnose diabetes by checking glucose levels in a blood test, which can be measured using different tests.
Fasting Blood Glucose Test: The fasting plasma glucose (FPG) test measures blood sugar after an 8-hour fast, allowing providers to monitor baseline blood sugar levels.
Random blood glucose test: The “random” option allows for the test to be administered at any time, regardless of whether the individual has fasted.
HbA1C: The HbA1C or glycated hemoglobin test provides an average blood glucose level over the past two to three months.
Glucose tolerance test: Doctors typically order an oral glucose tolerance test to screen for and diagnose gestational diabetes. It checks blood sugar after fasting overnight, after consuming a sugary drink, and after re-testing after 1 hour and 2 hours, identifying gestational diabetes if any readings indicate high blood sugar.
Treatment and Management:
Blood sugar monitoring:
Monitoring blood sugar levels is crucial for assessing the effectiveness of your diabetes treatment plan. It provides daily and sometimes hourly information on managing diabetes. The aim is to maintain normal blood sugar levels to prevent complications. Pre-meal blood sugar should be between 80–130 mg/dL, and after-meal levels should be no higher than 180 mg/dL two hours after eating.
Diet:
Consuming the right foods can manage blood sugar levels and help lose excess weight. Carb counting is crucial in diabetes, and a dietitian can assist in determining the appropriate carbohydrate intake. Small, daily meals with healthy foods like fruits, vegetables, whole grains, lean protein, and healthy fats are recommended. Certain foods can hinder blood sugar management efforts. A balanced diet is crucial for both mother and baby during gestational diabetes, preventing diabetes medication use. Healthy eating habits also help manage weight and reduce heart disease risk.
Exercise:
Exercise is crucial for diabetes management, as it helps cells react more effectively to insulin, lowering blood sugar levels and increasing insulin sensitivity. Maintaining a healthy weight, blood pressure and cholesterol can reduce the risk of diabetes-related health complications.
For type 1 or type 2 diabetes, aim for at least 150 minutes of moderate-intensity exercise weekly. For gestational diabetes, start slowly and gradually increase activity levels over time.
Oral diabetes medications: Oral diabetes medications, such as metformin, help manage blood sugar levels in Type 2 diabetes and prediabetes patients, as well as gestational diabetes patients.
Insulin: Type 1 diabetes patients require synthetic insulin injections for managing their condition. Some people with Type 2 diabetes also require insulin. Different types of synthetic insulin work at different speeds and durations in the body. The four main methods for taking insulin include injectable syringes, insulin pens, pumps and rapid-acting inhaled insulin.
References:
Harvard School of Public Health
Centers for Disease Control and Prevention
National Institute of Diabetes and Digestive and Kidney Diseases
Merck Manual: Consumer Version

